Femoracetabular Impingement Syndrome: A Quick Reference
What Is It?
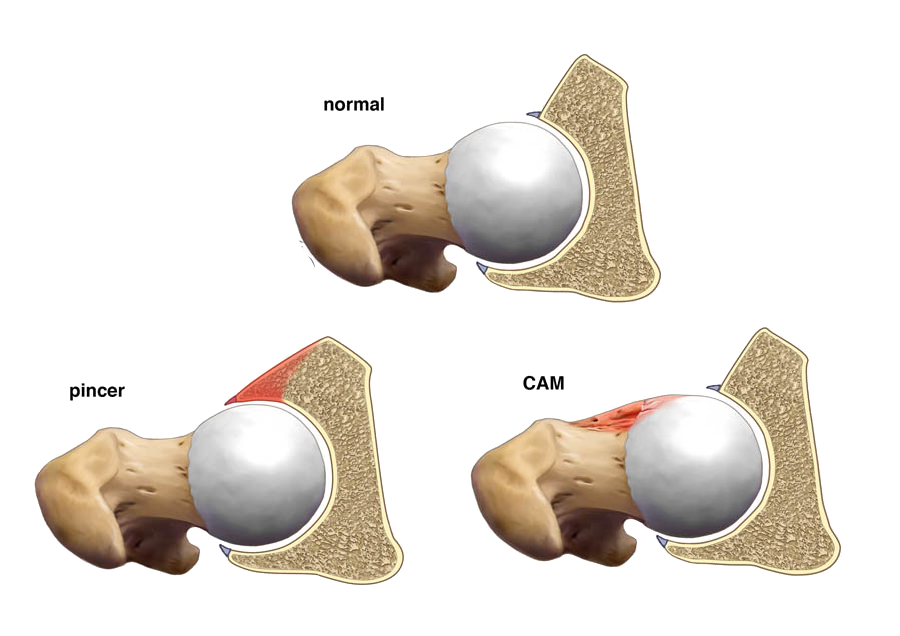
Femoracetabular Impingement Syndrome (FAIS, or often referred to as FAI) was defined by the Warwick Agreement as “a motion-related clinical disorder of the hip with a triad of symptoms, clinical signs and imaging findings. It represents symptomatic premature contact between the proximal femur and acetabulum.” [5]
Who Gets It and Why?
Individuals with FAIS have some form of morphological changes of the hip. However, the presence of either cam or pincer morphology is not necessarily indicative of FAIS. Cam morphology is significantly more common in men than in women, and it is also more prevalent in athletes than in the general population. Pincer morphology has been reported by some researchers to be relatively equal in prevalence between males and females, but other researchers have found it to be slightly more common in females. It has also been reported that it is more common for individuals to have a combination of cam and pincer morphology rather than one or the other. [1.2.3.5,9]
Casartelli and colleagues speculated that poor dynamic control of the hip joint may contribute to the development of FAIS. In support of their theory, they found that poor hip abductor strength was strongly correlated with poor movement pattern quality when evaluated by highly experienced physical therapists. [2]
Whether or not it is causative, weakness of hip muscles is commonly found in FAIS:
- Casartelli et al. (2011) found decreased hip flexion, adduction, abduction, and external rotation strength in those with FAIS compared to healthy controls [3]
- Nepple et al. found that hip abduction strength was inversely correlated with alpha angles on radiographs (used to identify cam morphology)
- Nepple and colleagues also found that those with FAIS and labral tears had decreased hip abduction and flexion strength
- The same study found that hip flexion strength deficits were associated with decreased function, decreased hip flexion ROM, and larger labral tears [7]
- Individuals with FAIS were found to have a lower external rotation to internal rotation isometric strength ratios than healthy controls [4]
Differential Diagnosis
Other conditions to consider and rule out when diagnosing a patient with FAIS include (but are not limited to):
- Hip osteoarthritis
- Gluteal tendinopathy
- Iliopsoas tendinopathy
- Greater trochanteric bursitis
- Athletic pubalgia
- Femoral neck stress fractures
- Lumbar referral
Clinical examination
The Warwick Agreement concluded that symptoms, clinical signs, and imaging findings must all be present to diagnose FAIS. [5]
Symptoms include pain, usually in the hip or groin, with motion or particular positions (usually hip flexion with or without internal rotation). Pain may also be accompanied by mechanical symptoms (e.g. clicking or catching) and restricted range of motion. [3,5,7]
As is often the case, no special test been found to be capable of identifying FAIS on its own. However, a few special tests were found to have some limited diagnostic accuracy:
- The FABER (Flexion Abduction External Rotation) test: Positive Likelihood Ratio of 0; Negative Likelihood Ratio of 0.59
- The IROP (Internal Rotation Overpressure) test: Positive Likelihood Ratio of 1.11; Negative Likelihood Ratio of 0.11
- The Impingement Sign/FADIR (Flexion Adduction Internal Rotation) test (When assessing for reduced pain-free flexion ROM in internal rotation: Positive Likelihood Ratio of 1.55; Negative Likelihood Ratio of 0.73
- The Anterior Impingement (Flexion Abduction Internal Rotation) test: Positive Likelihood Ratio of 0; Negative Likelihood Ratio of 0.44 [8]
While not currently within the scopes of practice of most physical therapists, radiographs are recommended to identify the presence of cam or pincer morphology and to determine whether additional imaging (MRA, MRI, or CT) is needed to see three dimensional and soft tissue structures. Radiographs are used to measure the α angle for the presence of cam morphology and the cross-over sign and center-edge angle for the presence of pincer morphology. [5]
Treatment
There is a lack of evidence available on effective treatment of FAIS. The effectiveness of surgery for management of FAIS has recently been brought into question. In active military members with FAIS, there was no statistically significant difference in outcomes between those who underwent arthroscopic surgery and those who received physical therapy. Unfortunately, comparisons between groups were underpowered because of a large crossover from the patients in the physical therapy group to the surgery group. Additionally, the majority of both groups reported no significant improvement after two years. [6]
Despite the lack of compelling evidence for either route, both physical therapy and/or surgery are still the recommended treatment approaches. [5]
While broad and not backed up by evidence, the general guidelines for physical therapy treatment for FAIS include:
- Strengthening of deep hip external rotators, hip flexors, and hip abductors to improve dynamic control of the femoroacetabular joint. [1]
- Improvement in movement pattern quality with simple and complex tasks [2]
As with the treatment of any condition, it is important to assess and treat the individual impairments of the patient. For additional information on FAIS, I encourage to utilize the references listed below. Have additional insights? Please leave a comment!
References
- Casartelli NC, Maffiuletti NA, Bizzini M, Kelly BT, Naal FD, Leunig M. The management of symptomatic femoroacetabular impingement: what is the rationale for non-surgical treatment?. Br J Sports Med. 2016;50(9):511-2.
- Casartelli NC, Maffiuletti NA, Brunner R, et al. Clinical Rating of Movement-Pattern Quality in Patients With Femoroacetabular Impingement Syndrome: A Methodological Study. J Orthop Sports Phys Ther. 2018;48(4):260-269.
- Casartelli NC, Maffiuletti NA, Item-glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthr Cartil. 2011;19(7):816-21.
- Diamond LE, Wrigley TV, Hinman RS, et al. Isometric and isokinetic hip strength and agonist/antagonist ratios in symptomatic femoroacetabular impingement. J Sci Med Sport. 2016;19(9):696-701.
- Griffin DR, Dickenson EJ, O'donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169-76.
- Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic Surgery or Physical Therapy for Patients With Femoroacetabular Impingement Syndrome: A Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med. 2018;:363546517751912.
- Nepple JJ, Goljan P, Briggs KK, Garvey SE, Ryan M, Philippon MJ. Hip Strength Deficits in Patients With Symptomatic Femoroacetabular Impingement and Labral Tears. Arthroscopy. 2015;31(11):2106-11.
- Pacheco-carrillo A, Medina-porqueres I. Physical examination tests for the diagnosis of femoroacetabular impingement. A systematic review. Phys Ther Sport. 2016;21:87-93.
- Van klij P, Heerey J, Waarsing JH, Agricola R. The Prevalence of Cam and Pincer Morphology and Its Association With Development of Hip Osteoarthritis. J Orthop Sports Phys Ther. 2018;48(4):230-238.