Inside Your Toolbox: Dry Needling
With a variety of different tools within our toolbox, how does one determine which to use for a given patient? Let’s take a look at Mr. Adams.
Mr. Adams is a 56-year-old computer programmer who spends most of his day sitting at the computer desk developing new software. He enjoys riding his bike around the neighborhood but is mostly sedentary. He lives in a two story house with his wife and 15-year-old daughter. Mr. Adams is coming to the clinic because of chronic neck and back pain that has been bothering him for over a year. He has no idea where the pain has come from and wants it to go away. He describes the pain as dull and achy that gets worse while sitting for long periods of time and better when he sleeps on his back. Upon a structural inspection, you notice a definite forward head, rounded shoulders, increased thoracic kyphosis, and decreased lumbar lordosis. He presents with generalized back weakness and tight pecs. No neurological symptoms are present and a vertebral artery test is negative. His past medical history shows hypertension and type II SLAP lesion on the right shoulder that was surgically repaired five years ago.
Looking at his generalized symptoms and condition, Mr. Adams seems like a typical patient that you may encounter in the clinic. As therapists, we all have many different tools that we can use to address patients with back and neck pain (ie. Soft tissue mobilization, joint mobilizations, manipulation, cupping, active release technique, dry needling, etc.). The question is, which intervention techniques would work best for him? Because this topic is about dry needling, I’ll discuss some of the benefits that it can produce.
What is Dry Needling?
Dry needling is a technique used to treat painful neuromusculoskeletal, muscular, and other orthopedic signs and symptoms such as trigger points, adhesions, movement impairments, and scar tissue. It involves using a thin filiform needle to penetrate the skin in the area exhibiting symptoms. Dry needling can also incorporate the use of electrical stimulation to target deeper tissues. There are different proposed models that attempt to describe the mechanism by which dry needling works, but the idea is to reduce motor end-plate noise and acetylcholine release by eliciting a localized twitch response (LTR). These localized twitch responses may:
Normalize levels of inflammatory chemicals like bradykinin, calcitonin, gene-related peptide, and substance P.
Attract satellite cells to promote muscle regeneration in the area of microtrauma towards the affected tissue.
Cause mechanical deformation of collagen fibers that convert to electrical energy for tissue remodeling through the piezoelectric effect.
Dry needling can also cause muscle relaxation, as well as bring more blood flow towards the affected area. With these benefits, can everyone use this technique? Unfortunately not because certain states still prevent therapists from using it.
Certification
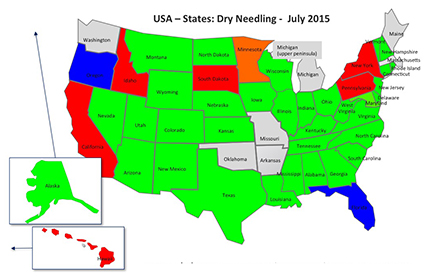
In order to utilize this tool, you must first be a licensed physical therapist or another approved healthcare practitioner. There are different courses that offer training in dry needling. The popular ones to which clinicians typically refer are Dr. Ma’s Integrative Dry Needling, Kinetacore, Myopain Seminars, and Spinal Manipulation Institute. Each one focuses on slightly different areas, so it’s important to understand which area you want to learn. For example, the Spinal Manipulation Institute course is taught by Dr. Dunning and covers dry needling and spinal manipulation, whereas Kinetacore is taught by Edo Zylstra and covers dry needling and pelvic function. It all depends on where your interests lie. Even with a license and certification in dry needling, your state must be approved to allow physical therapists to practice it. Currently (2015), here are the states that are approved for dry needling:
- Green and orange = states that are allowed to practice.
- Red = states that are currently not allowed to practice.
- Blue states = states that recently tried to get legislation passed but are not successful due to their state practice act.
Without diving too far into the details, there are huge debates between acupuncturists and physical therapists about the use of dry needling. Part of the reason is due to what is written within each state practice act and how the wording can be used against therapists using dry needling. Other parts involve keeping the practice of using a needle to penetrate the skin within acupuncture only. There are also safety concerns that other professionals worry about. Some of the contraindications and precautions for dry needling involve bloodborne pathogens, puncturing the lungs, pregnancy, high doses of anticoagulants, cardiac pacemakers, and others (See table below for more). In any case, physical therapists are becoming allowed to practice this technique in more and more states.
What does the Research Say?
There is minimal research out pertaining to dry needling and the strength of some of the articles is limited. In 2005, Furlan et al looked at acupuncture and dry-needling for low back pain. Within this systematic review, they determined that dry needling can be an effective adjunct to other therapies for chronic low back pain. Another systematic review written by Kietrys et al in 2013 showed that dry needling can immediately decrease pain in shoulder, neck, and upper extremity patients with myofascial pain syndrome. With these different articles, is it safe to say that dry needling is the sole treatment solution for patients? Absolutely not! More research is needed to determine if dry needling is more effective than standard physical therapy care alone and which patient population will benefit most from it.
Based on my experiences with observing dry needling, it appears to be an effective adjunctive therapy when combined with other tools utilized within physical therapy. So after all that information thrown at you, let’s go back to the initial case with Mr. Adams. Do you think dry needling alone is effective enough to help him? Do you think dry needling is even necessary for Mr. Adams? With all said and done, there are many different approaches that you can use to treat Mr. Adams and it’s important to understand that any of those interventions may be part of the solution. There is no “one” solution for any patient. As long as we are competent with our abilities to treat patients and listen to what the patient has to say and continue to reassess how the patient responds to our treatment, then there is no doubt that the tools that we decide to use will be the correct tools for their treatment.
| Precautions | Contraindications |
|---|---|
| Thoracic Spine and lung field | Inadequate practical knowledge |
| L2 and Kidneys | Consent - denied by patient |
| Iliac crest - too perpendicular and too lateral = viscera | Local infection |
| Sacral / Coccyx | Bleed disorders |
| Local Skin lesions | Pregnancy |
| Patients with a needle aversion or phobia may object | Compromised equipment |
| Patients with significant cognitive impairment | Over a joint replacement, breast implant or cardiac pacemaker |
| Patients unable to communicate directly | Scalp areas of infants |
| Neurovascular bundles associated with the | Immune-suppressed patients |
| Femoral Triangle | Nipples, umbilicus and external genitalia |
| Cubical Fossa | Over rib cage or over a rib (Level 2) |
| Popliteal Fossa | Spinal cord stimulators and other implants |
| Supra-clavicular triangle | Patients allergic to nickle or chomium |
References:
- RULINGS ABOUT DRY NEEDLING BY U.S. STATE BOARDS. (2015). Retrieved October 1, 2015
- State Training Guidelines - Integrative Dry Needling. (n.d.). Retrieved October 1, 2015
- Mcpartland JM. Travell trigger points--molecular and osteopathic perspectives. J Am Osteopath Assoc. 2004;104(6):244-9.
- Unverzagt C, Berglund K, Thomas JJ. DRY NEEDLING FOR MYOFASCIAL TRIGGER POINT PAIN: A CLINICAL COMMENTARY. Int J Sports Phys Ther. 2015;10(3):402-18
- Painful and tender muscles: dry needling can reduce myofascial pain related to trigger points muscles. J Orthop Sports Phys Ther. 2013;43(9):635.
- Dommerholt J, Moral OM, Grobli C. Trigger point dry needling. J Man Manip Ther. 2006;14(4):70-87
- Description of dry needling in clinical practice: An educational resource paper. APTA. 2013.
- Cotchett MP, Landorf KB, Munteanu SE. Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: a systematic review. J Foot Ankle Res. 2010;3:18.
- Furlan AD, Van tulder M, Cherkin D, et al. Acupuncture and dry-needling for low back pain: an updated systematic review within the framework of the cochrane collaboration. Spine. 2005;30(8):944-63.
- Kietrys DM, Palombaro KM, Azzaretto E, et al. Effectiveness of dry needling for upper-quarter myofascial pain: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2013;43(9):620-34.